The economic costs of smoking
In 2017, the total health costs – or direct costs – related to smoking exceeded CHF 3 billion.
In the same year, estimates show indirect costs to the economy, due to productivity losses, of up to CHF 3.1 billion.
Direct and indirect costs related to smoking account for more than half of all the economic costs linked to addictions in Switzerland.
In addition to the very significant human costs described in our page, Mortality and Morbidity Related to Smoking, tobacco consumption entails substantial economic and social costs for society. At the economic level, it is usual to quantify this burden by estimating, on the one hand, the direct costs to the health system caused by the medical care of patients with tobacco-related diseases and, on the other hand, the indirect costs to the economy due to productivity losses linked to short- or long-term sick leave, loss of work capacity, and deaths.
Estimates for the year 2017
A study commissioned by the Federal Office of Public Health produced various estimates of the economic costs related to addictions (Fischer et al., 2020[1]). It estimates that all health costs related to smoking, so-called direct costs, exceeded CHF 3 billion in 2017 (Figure). Estimates of indirect costs to the economy due to productivity losses are also proposed by considering different assumptions of the effects of illness (morbidity) or death (mortality) on productivity. Various assumptions are made about the impact of illness (morbidity) or death (mortality) on productivity. Estimates based on the concept of Human Capital (HC)[2] costs indicate that the economy had to bear additional costs of CHF 3.1 billion in 2017. Calculations that assume that a sick or deceased person can be replaced after a certain period of time by a new (e.g. until then unemployed) worker, and that only take into account the productivity losses during these so-called friction periods (hence the term friction costs, FC, or friction cost approach, FCA), yield much lower figures: Tobacco-related costs are estimated at CHF 833 million. By adding the direct and indirect costs, the total annual costs related to tobacco consumption in Switzerland are estimated at more than CHF 6.1 billion for the HC calculation method, and at nearly 3.9 billion for the FC method.
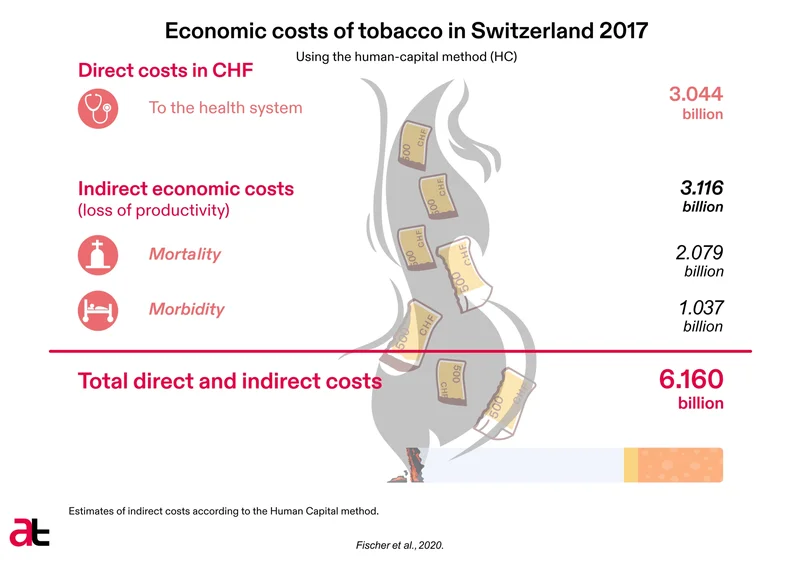
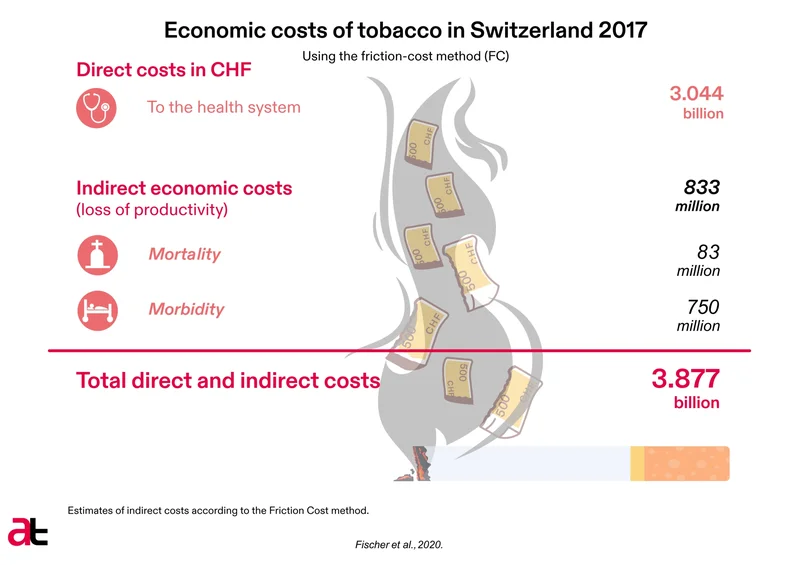
Figure: Economic costs related to tobacco in Switzerland in 2017, in millions of francs. *HC/FC: estimates of indirect costs according to the Human Capital, HC, and Friction Cost, FC, methods. (Source Fischer et al., 2020[3])
Contribution of smoking to the total economic costs of addictions
If we consider the costs of tobacco use in relation to those of alcohol and illegal drugs, the share of direct and indirect tobacco costs represents some 54% [4] of the total costs of addictions, according to the Human Capital calculation method, or 51%[5] of the total costs using the Friction Costs method (or 49% if the estimated costs of gambling are also considered[6]).
Previous economic and social cost estimates
A previous study of the year 2015 (Mattli et al., 2019[7]) estimated direct medical costs of CHF 3 billion (CHF 363 per capita/total population) and indirect loss of productivity costs of CHF 2 billion (CHF 242 per capita/total population). The CHF 3 billion in medical costs described in this study corresponded to 3.9% of all 2015 health expenditures in Switzerland.
The first estimates of the costs of smoking in Switzerland date from the end of the 1990s (Vitale et al., 1998[8]). Based on methodologies significantly different from the estimates presented above, they revealed direct costs of CHF 1.2 billion, indirect costs of CHF 3.8 billion, and human costs approaching CHF 5 billion. The latter human costs are thought to be intangible (they are derived from estimates of the value attached to a reduction in the quality of life in the event of illness, the consequences of death, etc.) and are generally no longer considered in cost estimates related to smoking; we consequently no longer estimate social costs, but rather economic costs.
It should be noted that estimates related to the costs of passive smoking were produced in the late 2000s (Hauri et al, 2009[9]). According to these estimates, the direct and indirect costs due to passive smoking totalled CHF 252 million in 2006.
Global economic costs of smoking
Estimates of ‘global’ economic costs have also been derived by assessing the total economic cost of tobacco-attributable disease in 152 countries, representing 97% of smokers worldwide (Goodchild et al., 2018[10]). The results show that in 2012, the global cost of smoking in terms of health care (direct costs) reached USD 422 billion, or no less than 5.7% of health expenditure at the global level; with direct costs appearing proportionally higher in high-income countries. Indirect costs were estimated at USD 357 billion for morbidity and USD 657 billion for mortality. Altogether, these estimates put the total economic costs of tobacco use at USD 1.4 trillion for 2012, which represents 1.8% of annual global GDP for that year. At the Swiss level, the estimates for 2017 presented above show total costs (direct and indirect) representing between 0.6%[11] (Friction Costs method) and 0.9%[12] (Human Capital method) of GDP. This discrepancy with global estimates is hardly surprising given Switzerland's very high per capita GDP.
Importance of monitoring the economic costs of smoking
To date, no real systematic monitoring has been undertaken to assess the economic costs of smoking in Switzerland. This has led to problems of comparability between the various estimates proposed in recent decades. However, in order to manage smoking prevention at the national level, it seems essential to consider cost monitoring as a key element of the surveillance system. To do so necessitates the use of a validated and replicable methodology. Ideally, the standardised methodology defined for this should allow cost modelling over the coming decades, including on the basis of various assumptions or regulatory models. At the level of direct health costs, these models – estimates and projections – should ideally also be available by type of disease (costs linked to lung cancer, other types of cancer, or ischemic heart disease). Also, the preferred methodologies should be able to be updated without great delay to allow for adjustment of estimates and projections based on the evolution of the market. For example, the arrival of new products must be accounted for, including lost productivity; scientific evidence on their harmful effects; and related clinical aspects, such as the impact on treatment costs. An alignment, or comparison with certain tools and principles issued by the WHO through its “Toolbox on the evaluation of the economic costs of smoking” would also be welcome (World Health Organization, 2011[13]).
Finally, it should be noted that other indirect, or external, costs related to smoking behaviour are generally omitted from the proposed estimates and should be given more attention in the future. We are thinking in particular of the costs of collecting and treating waste (e.g. cigarette butts, which are a form of toxic plastic, but also the batteries of Puff Bars and other disposable e-cigarettes or electronic nicotine delivery systems). We must also consider the environmental impact of producing tobacco products, and the pollution the waste causes when dropped as litter into public spaces or into nature. The entire production cycle of the billions of cigarettes consumed annually in Switzerland involves significant outsourcing, as tobacco is often grown, processed, and manufactured elsewhere. This should be taken into account in a comprehensive cost assessment.
[1] Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[2] A method that accounts for all the work time lost due to illness or death and based on the assumption that a person who dies or is unable to work as a result of illness cannot be replaced due to a tight job market.
[3] Tableau 1 p. 19 et Tabelle 37 p. 105; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[4] Tabelle 38, page 106 ; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[5] Tableau 2, page 19 ; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[6] Tableau 1, p. 19 ; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[7] Mattli, Renato; Farcher, Renato; Dettling, Marcel; Syleouni, Maria-Eleni; Wieser, Simon (2019): Die Krankheitslast des Tabakkonsums in der Schweiz: Schätzung für 2015 und Prognose bis 2050. Download.
[8] Vitale, Sarino; Priez, France; Jeanrenaud, Claude (1998): Le coût social de la consommation de tabac en Suisse. Download.
[9] Hauri, D.; Lieb, C.; Kooijman, C.; Wenk, S.; van Nieuwkoop, R.; Sommer, H.; Röösli, M. (2009): Gesundheitskosten des Passivrauchens in der Schweiz. Download.
[10] Goodchild, M.; Nargis, N.; Tursan d'Espaignet, E. (2018): Global economic cost of smoking-attributable diseases. Tob Control. 2018 Jan;27(1):58-64. Download.
[11] Table 2, page 19; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[12] Tabelle 38, page 106; Fischer, Barbara; Mäder, Béatrice; Telser, Harry (2020): Volkswirtschaftliche Kosten von Sucht. Download.
[13] World Health Organization (2011): Economics of tobacco toolkit: assessment of the economic costs of smoking. Download.
AT Switzerland, June 2023